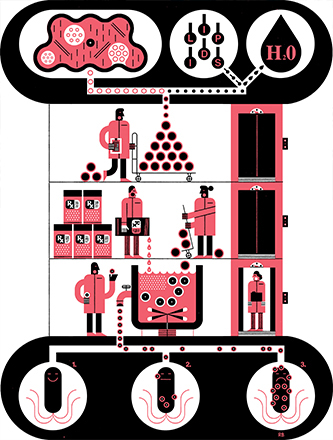
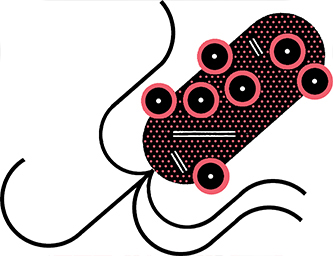
Bacterial infections can take hold in the body when a pathogenic, or disease-causing, microorganism enters and delivers toxins to healthy human cells. One way bacteria accomplish this is by releasing vesicles, which act as tiny envelopes transporting toxins and other virulence factors―molecules that help infection take hold―to host cells. The virulence factors allow the bacteria to effectively infect healthy human cells and make people sick.
The rapid emergence of antibiotic-resistant bacteria―bacteria that do not respond to currently available antibiotic treatment―is a worldwide problem that is only expected to worsen. The Centers for Disease Control and Prevention (CDC) estimates that almost three million people in the U.S. develop antibiotic-resistant bacterial infections each year, with more than 35,000 dying as a result. Developing new antibiotic drugs is a long and expensive process and not widely seen as an effective long-term solution. Anti-virulence strategies that seek to disarm bacteria’s virulence factors are one possible approach.
“The idea of an anti-virulence strategy is to eliminate those virulence factors or inhibit the function of those so the bacteria don’t have those advantages,” says Angela Brown, an associate professor of chemical and biomolecular engineering whose research has focused on anti-virulence strategies. “Then the immune system could have time to clear the infection before it takes hold.”